
When Is Dental Bone Grafting Necessary for Successful Implants? Clear Guidelines for Candidates and Procedures
If you lack enough jawbone from tooth loss, gum disease, or injury, a bone graft often becomes necessary so an implant can have a stable, long-lasting foundation. A bone graft rebuilds missing bone so the implant can fuse securely and reduce the risk of implant failure.
You will learn how grafting works, when your dentist will recommend it, and what risks and results to expect. This article will help you decide if grafting is likely part of your path to a successful implant and what steps follow if it is.
Understanding Dental Bone Grafting
You will learn what bone grafting means, the main graft types, and how grafts support implants. This helps you know why a dentist might recommend grafting and what to expect.
What Is Dental Bone Grafting?
A dental bone graft in Woodbury adds bone or bone-like material to your jaw where bone is thin or missing. Your dentist places the graft during a minor surgery to build height, width, or density.
Graft material can come from your own body, a donor, an animal source, or a lab-made material. The graft acts as a scaffold. Over months, your own bone grows into that scaffold and becomes stronger.
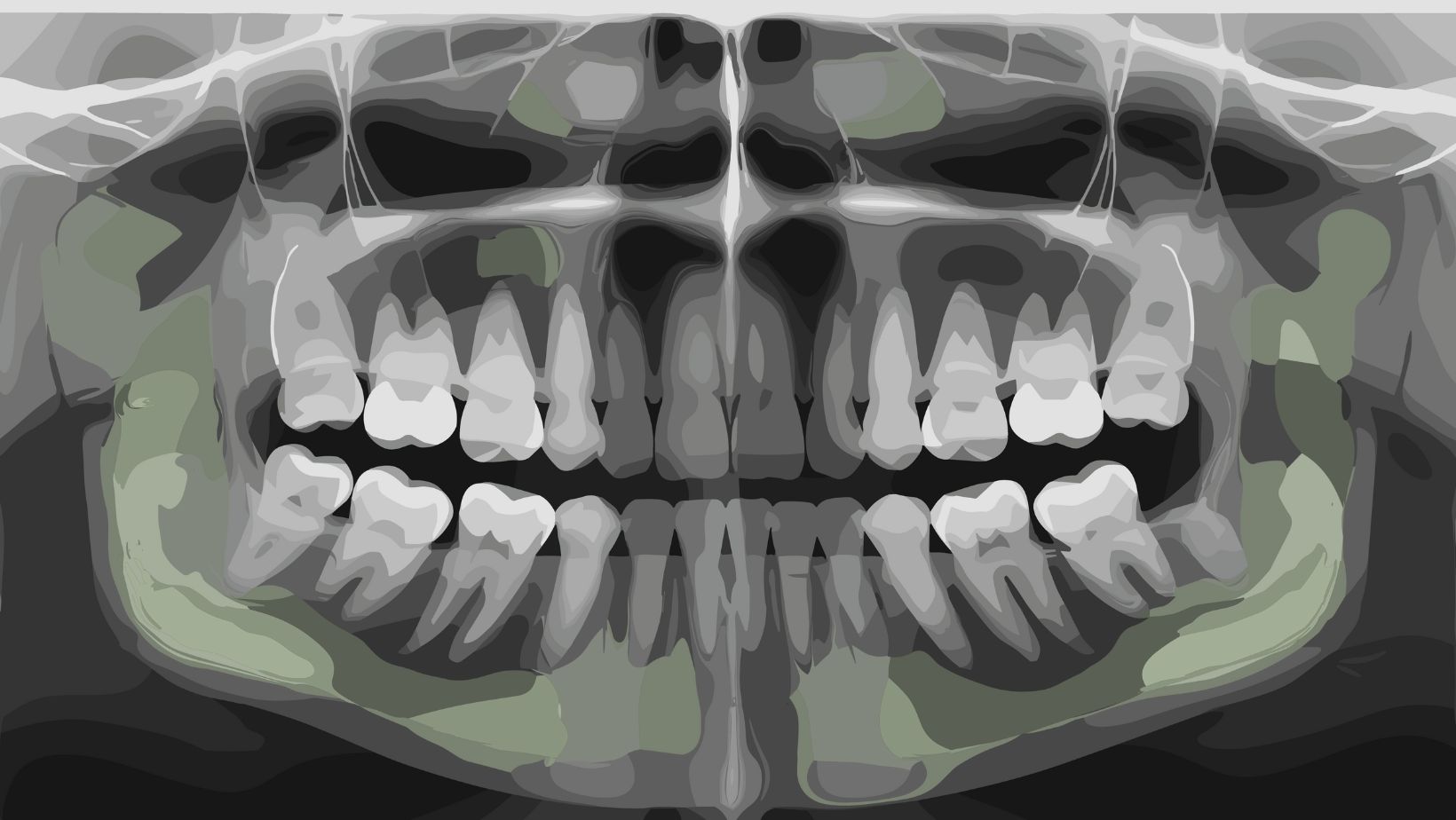
You may need a graft after tooth loss, long-term denture wear, infection, or trauma. Your dentist will use X-rays or a CT scan to measure bone and plan the graft.
Types of Bone Grafts
Autograft: bone taken from another part of your body, often the chin or hip. It has the best chance to fuse because it contains your living cells.
Allograft: human donor bone from a tissue bank. It avoids a second surgical site and works well for many patients.
Xenograft: bone from an animal, usually bovine. It provides a strong scaffold but may resorb more slowly.
Synthetic grafts: lab-made materials like calcium phosphate or bioactive glass. They are safe, sterile, and predictable.
Common procedures include:
- Ridge augmentation to widen a jaw ridge.
- Sinus lift to add bone under the sinus in the upper back jaw.
- Socket preservation to keep bone after tooth extraction.
The Role of Bone Grafting in Implant Dentistry
Bone grafting creates the volume and strength implants need to fuse with your jaw. Implants require enough bone to hold the titanium post steady during healing.
Without enough bone, implants can tilt, loosen, or fail over time. Grafting lowers these risks by improving support and positioning for the implant.
Your dentist will decide timing based on your case:
- Immediate grafting at extraction in some situations.
- Delayed grafting if infection or severe bone loss exists. They will also plan healing time, which can range from a few months up to six months before implant placement.
When Dental Bone Grafting Is Necessary for Implants
You need enough jawbone width, height, and strength for an implant to fuse and stay stable. The sections below explain how clinicians check bone, why bone is lost, when grafts are placed, and clear signs that you likely need grafting.
Assessing Bone Volume and Density
Dentists use 3D imaging like a CBCT scan to measure your jaw in millimeters. They check bone height (from sinus or nerve to crest), width (buccal to lingual), and density (quality of bone) to decide if an implant will be stable.
If the ridge is less than about 6 mm wide or there’s under 10 mm height to key landmarks, surgeons often plan a graft. Bone quality matters too: soft, low-density bone raises risk of implant failure even if dimensions look okay.
Physical exam also matters. Your clinician will probe the ridge, look at soft tissue, and review medical history. Smoking, uncontrolled diabetes, and medications that affect bone change the judgment about whether grafting is necessary.
Common Causes of Bone Loss
Tooth loss quickly leads to bone shrinkage where the tooth root used to be. Without the root stimulating the jaw, bone can resorb vertically and horizontally over months to years.
Periodontal disease destroys the bone around infected teeth, often leaving uneven bone defects. Severe infections, cysts, or trauma can remove chunks of bone too, making implant placement impossible without grafting.
Sinus expansion (pneumatization) after upper molar loss reduces vertical height beneath the sinus. Long-term denture wear can flatten the ridge. Certain medical conditions and some medications also speed bone loss.
Timing of Grafting Procedures for Implant Success
You may get a graft before implant placement, at the same time as the implant, or after a failed implant. The choice depends on how much bone is missing and the type of graft used.
If you need large volume gain or vertical height, clinicians often graft first and wait 4–6 months for consolidation. For small horizontal defects, a simultaneous graft-and-implant approach often works and shortens total treatment time.
Sinus lifts usually occur before or during implant surgery depending on residual height. Your surgeon will factor healing time, graft material (autograft, allograft, xenograft, or synthetic), and your health when setting a timeline.
Indicators for Bone Grafting Prior to Implant Placement
You should expect a graft if CBCT shows insufficient width (<6 mm) or height under anatomical limits (sinus floor or inferior alveolar nerve). Large defects from extractions or infections also point to pre-implant grafting.
Visible ridge collapse, thin gingival tissue overlying bone, or exposed implant threads on trial placement are clinical hints you’ll need more bone. Failed previous implants or widespread periodontal bone loss are strong indicators too.
If you smoke, have osteoporosis, or take medications that affect bone healing, your surgeon may recommend grafting or modify the plan to improve long-term success.
Risks, Considerations, and Outcomes of Bone Grafting
Bone grafting can add strength and volume to your jaw, but it also brings possible complications, a recovery period, and variable success rates. Know the common risks, realistic prognosis, and what to expect day to day after the procedure.
Potential Risks and Complications
You can expect normal swelling, bruising, and mild pain for several days after grafting. Infection is a key risk; signs include increasing pain, pus, fever, or bad taste. Your surgeon may prescribe antibiotics to lower this risk.
Graft failure can happen if the graft does not integrate with your bone. Smoking, uncontrolled diabetes, poor oral hygiene, and low blood flow raise that risk. Rarely, nerves or sinus membranes can be damaged during surgery, causing numbness or sinus problems.
Bleeding is usually minor but can be more serious if you take blood thinners. Rejection of donor material is uncommon, yet allergic or immune reactions can occur with some graft types. Talk to your dentist about specific risks tied to your health and the graft material.
Success Rates and Prognosis
Most dental bone grafts succeed when you follow post-op care and your health is stable. Autografts (your own bone) typically show the highest success, followed by allografts and synthetic materials. Your surgeon will choose the best option based on defect size and location.
Success often means enough bone forms to place an implant in 3–9 months, depending on graft type and jaw location. Smoking and certain medical conditions can cut success rates significantly. If a graft fails, your clinician may repeat the graft or use alternative techniques.
Long-term implant survival after a successful graft matches implants placed in native bone if you maintain oral hygiene and regular dental visits. Expect your clinician to monitor graft healing with X-rays and exams before implant placement.
Recovery Timeline and Patient Experience
Day 0–7: Expect swelling, mild to moderate pain, and limited eating. Use cold packs, soft foods, and prescribed pain relievers. Keep the surgical site clean but avoid vigorous rinsing.
Weeks 2–8: Swelling and bruising decline. Stitches often come out or dissolve. You may return to normal activity, but avoid hard chewing in the graft area. Follow any dietary limits your clinician gives.
Months 3–9: Bone integrates and strengthens. Your dentist will use X-rays to confirm graft maturity. Once the graft is stable, they place the implant. Full return to normal chewing can take several more months after implant placement.
Practical tips: stop smoking before surgery, control chronic conditions, and follow medication and care instructions closely to improve comfort and outcomes.





